Knee Osteotomy
Diet
- Start with clear liquids (jello, soup broth, Gatorade, etc.), crackers, white bread and other light foods
- Progress slowly to heavier foods as you tolerate the lighter foods without any nausea
Wound Care
- Keep your dressing clean and dry and in place for four days after surgery.
- You may shower by placing a large garbage bag over your dressing and brace – do not submerge your leg under water
- On day 4 after surgery, you may remove your dressing. It is normal for there to be some blood staining on the dressings. If the wounds are completely dry, you may just place band-aids over them. If there is a small amount of drainage still coming from the wounds, place a clean and dry dressing on them daily until the drainage stops. If the drainage continues, call Dr. Roth’s office to inform him.
- Once the incisions are completely dry for 24 hours, you may shower. Let the water and soap run over the incisions and pat them dry with a clean towel after the shower. Do not scrub the incisions or vigorously dry them. Do not submerge the incisions under water (e.g. NO bath tubs, swimming pools, hot tubs, ocean swimming, etc.).
Medications
- You will usually have a nerve block which will last for 8-16 hours after surgery. You will start to feel some tingling in your knee and your foot when the nerve block starts to wear off. This is the sign that the pain is soon to follow, so you want to start taking your pain medication at this time
- Studies have suggested that Non-Steroidal Anti-Inflammatory medications (NSAIDs) may impair or inhibit tendon healing. If at all possible, it is best to try to avoid NSAIDs for a period of 2 weeks after surgery.
- You have been given a prescription at your preoperative visit for narcotic pain medications (OxyCODONE, Percocet, Norco, etc.). Dr. Roth may have given you a long acting medication (OXYCONTIN) which is to be taken twice per day for the first three days after surgery only. You can take this medication at 8pm the night of your surgery. You have also been given a short acting medication (e.g. Percocet) which should be taken as soon as you start to feel some tingling in your toes or any suggestion of pain.
- If you have a history of Obstructive Sleep Apnea (OSA), be sure to let Dr. Roth know as he may decide to change your post-operative pain regimen.
- If your narcotic pain medication has ACETAMINOPHEN in it (e.g. Norco, Percocet) then you cannot also take TYLENOL, which is the same medication.
- Side effects of the pain medication include nausea, vomiting, dry mouth, constipation, dizziness and lightheadedness. Taking the medication with food will decrease the risk of nausea. For constipation, it is recommended that you take a stool softener while taking the narcotic. Colace can be purchased over the counter. Take one tab 2-3 times per day.
- Try to wean off of the narcotic pain medication as soon as possible. Adding in NSAIDs (e.g. Advil 600 mg 4 times per day OR Aleve 440 mg twice per day) at two weeks after surgery will help you transition away from the narcotic medications. Fibrous tissue has organized by then so NSAIDs will no longer affect tissue healing.
- Dr. Roth’s Suggested Post-Operative Pain Management Regimens (Percocet and oxyCONTIN used as an example, but be sure to confirm which medication has been prescribed by Dr. Roth) OxyCONTIN is typically only prescribed for the first three days after surgery. After that, just continue with the Percocet.
Suggested Pain Regimen 8 AM 1 OxyCONTIN (if prescribed)
+
Pain Level 0-2: NO Percocet
Pain Level 3-6: ONE Percocet
Pain Level 7-10: TWO Percocet12 PM (NOON) Pain Level 0-2: NO Percocet
Pain Level 3-6: ONE Percocet
Pain Level 7-10: TWO Percocet4 PM Pain Level 0-2: NO Percocet
Pain Level 3-6: ONE Percocet
Pain Level 7-10: TWO Percocet8 PM 1 OxyCONTIN (if prescribed)
+
Pain Level 0-2: NO Percocet
Pain Level 3-6: ONE Percocet
Pain Level 7-10: TWO Percocet12 AM (MIDNIGHT) Pain Level 0-2: NO Percocet
Pain Level 3-6: ONE Percocet
Pain Level 7-10: TWO Percocet4 AM (IF NEEDED) Pain Level 0-2: NO Percocet
Pain Level 3-6: ONE Percocet
Pain Level 7-10: TWO Percocet - Do NOT drive a car or operate any heavy machinery while you are taking narcotic pain medication (OxyCODONE, Oycontin, Norco, Percocet, Tylenol #3, etc.)
Activity
- It is very important to try to make sure that the knee is able to get fully straight after any knee reconstruction surgery. In order to avoid the knee become stuck in a bent position, do not place pillows behind then knee, but rather place pillows under the ankle/foot, which will force the knee into full extension. This will likely be uncomfortable, but will NOT damage the repair.
- Use crutches to assist with walking and help provide you stability as you learn to walk on an injured extremity. Wear your brace when walking. For the first two weeks after surgery, your brace should be locked in full extension whenever you are walking. For the first six weeks after surgery, your weight bearing should be “Toe-Touch Weight Bearing,” meaning you are just allowed to put enough weight to touch the foot to the ground for some balance while walking
- Your weight bearing will be advanced after six weeks.
- You may have bene given a Continuous Passive Motion machine (CPM). If you were, the CPM is to be used approximately 4 hours per day. It is OK to sleep in this machine. Start the machine on the first day after surgery at 30 degrees and advance by 10 degrees per day. Once you get to 100 degrees, you may call the company and return the machine.
- When you are not in the CPM machine and are laying down, elevate the operative extremity to chest level whenever possible to decrease swelling
- You are to walk with crutches at all times
- If you had a MENISCUS REPAIR, do NOT bear more than 50% of your weight on the operative leg. Do NOT bend the knee past 90 degrees.
- Avoid long periods of sitting with the leg below your waist or long periods of standing/walking for the first 7-10 days after surgery as these activities are likely to increase the swelling of your leg.
- You may return to sedentary work / school 3-4 days after surgery if swelling and pain are tolerable and you are no longer taking narcotic pain medications.
- DO NOT SMOKE cigarettes, smokeless tobacco, cigars, dip, chew, or any other tobacco product for at least 3 months after surgery if at all possible, as these will all inhibit healing of the repair, increase the risk of infection, and decrease the ability of the wound to heal.
Brace
- Brace is to be worn at all times (day and night) locked fully straight for the first week after surgery except when showering, doing exercises or when you are using the CPM. The brace will be unlocked by Dr. Roth when appropriate.
ICE Therapy
- Dr. Roth highly recommends purchasing an ice machine for the post-operative period as it is much more convenient than ice packs, however, if necessary, ice packs are sufficient as well.
- Start ice immediately after surgery. You will have a bulky dressing on your knee and therefore you may not feel like the cold is penetrating, but it is still helping.
- Ice for 20 minutes a minimum of four times daily, or more often if you prefer, but no more often than 20 minutes every hour. Be sure there is always something between the ice pack and your skin and do NOT ice for longer than 20 minutes at a time or you could get frostbite.
- If you had a block at the time of surgery, your leg may be numb for up to 24 hours. It is particularly important during this time to be aware of the clock when you are icing as you will not feel the cold and frostbite is a real concern.
Exercise
- You may start your exercises 24 hours after surgery (described below).
- Try to do your exercises a minimum of 3 times per day after surgery.
- Your knee will feel painful and stiff after surgery which is normal, but it is appropriate and healthy to start trying to bend and straighten it (unless otherwise instructed by Dr. Roth)
- Your goal range of motion at your first post-operative visit is to be able to get the knee completely straight and to 90 degrees of flexion.
- Formal physical therapy will begin after your first post-operative visit.
- Do ankle pumps throughout the day to minimize the risk of blood clots.
Specific Exercises
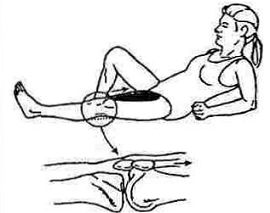
Quadriceps Sets
Lie down or sit with your leg fully extended. Tighten and hold the muscle on the front of your thigh (“quad”) to make the knee flat and straight. Think about pushing the back of your knee down against the bed or floor. If you are doing it correctly, the knee will flatten and the kneecap will slide up toward the thigh muscle.
Heel Props
Lie on your back with your heel propped on a rolled towel or on the armrest of a couch. Or, sit in a chair with the heel propped on a chair. Leave nothing behind the back of your knee (e.g. no pillows behind your knee) and let the knee relax and become straighter. If you are unable to get the knee straight like this, you can place a weight (2 to 5 lbs.) on the thigh, just above the kneecap, to help push the knee straight. Patients often worry about “hyperextending” the knee, but this does not need to be worried about as long as you are not using more than 5 lbs. of weight.
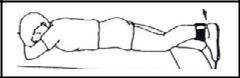
Prone Heel Hangs
Lie on your stomach on a raised surface such as a table or a bed, and slide down so that your knee at the edge of the table and your foot is off the edge. Let the knee relax and let gravity pull your knee straight. As in the Heel Props above, if you cannot get the knee straight, a light weight (2 to 5 lbs.) can be hung from your heel to help add to the pull of gravity.
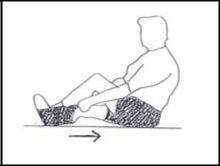
Heel Slides
While sitting or lying on the floor or a bed, gently try to slide your heel along the floor toward your thigh by bending your knee. Hold this for a few seconds, and then slowly straighten the knee back out. If you have trouble doing this, you can take a towel and wrap it around the ball of your foot and use your hands to help gently pull your knee into flexion.
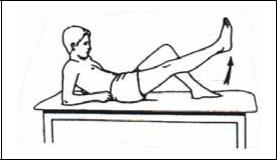
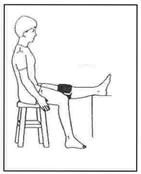
Straight Leg Raises
If your knee bends when you are doing this exercise, you are not yet ready. Continue working on the QUADRICEPS SETS (described above) until you are able to do this exercise keeping the knee completely straight
The Straight Leg Raise is all about focusing on tightening your quadriceps muscle, which is why you have to be good at the Quad Set before you can be good at the Straight Leg Raise
- The steps of a good Straight Leg Raise are as follows:
- Tighten the quadriceps as much as you can (same as a quad set)
- Tighten it even harder!
- Lift your heel 4 to 6 inches off the floor, keeping the knee straight
- Think about tightening your quad even harder!
- Lower the leg gently back to the floor, keeping the quad as tight as possible
- Try one more time to tighten the quadriceps muscle
- Now relax and rest a minute or two, and repeat
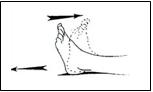
Ankle Pumps
Move your foot up and down like you are stepping on and off of a gas pedal. This helps circulate blood through your leg. Do this about 20-30 times, every few hours.
Emergencies
- During business hours, contact Sabrina in Dr. Roth’s office at 510-267-4013. If you are not getting through to Sabrina because she is busy in the office and not able to immediately answer the phone, contact the Webster Call Center at 800-943-8099 and they will track down Dr. Roth.
- For concerns that cannot be addressed during business hours, call the Webster Call Center at 800-943-8099.
- For the first 48 hours after surgery, the call center will put you through directly to Dr. Roth’s cell phone if you would like. Dr. Roth feels that it is very important that you have the opportunity to speak directly to your surgeon rather than to an “on-call” physician within the first 48 hours after surgery if you have concerns. Because Dr. Roth is typically at home with his family during these times, he would appreciate the use of discretion when taking advantage of this service. If you feel you have a simple question that you would be comfortable with the on-call physician handling, please inform the call center.
- Please contact Dr. Roth’s office immediately if any of the following are present, or for any other concerns:
- Pain that is not controlled by the regimen described above
- Pain that is unrelenting or getting worse over time rather than staying the same or improving
- Numbness that lasts longer than 24 hours after surgery
- Fever (greater than 101⁰ - low grade fever is normal for the first few days after surgery)
- Redness around the incisions
- Continuous drainage or bleeding from the incision (some drainage is expected)
- Difficulty breathing
- Chest Pain
- Light headedness or passing out o Uncontrollable nausea, vomiting
- Color change in the operative extremity o Blistering of the skin
- If you have an emergency that requires immediate attention, proceed to the nearest Emergency Room.
Follow-UP
- If you do not already have a follow-up appointment scheduled, please contact Dorothy at (510) 267-4016 to arrange an appointment. Follow-up appointments are generally 7-10 days after surgery.











